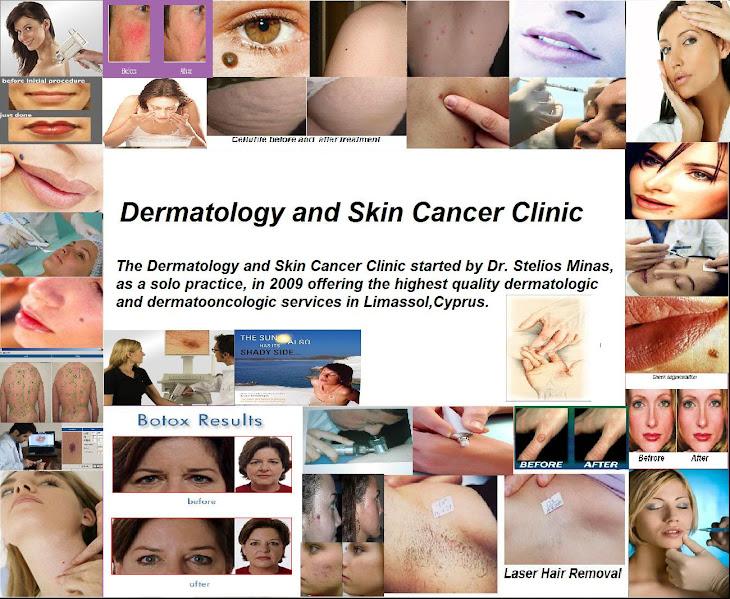
1.Antiaging 11.Allergology
2.Mycology 12. Dermatooncology
3.Venereology 13.Skin Cancer Screening
4.Adult Dermatology 14.Skin Augmentation
5.Pediatric Dermatology 15.Botox
6.Geriatric Dermatology 16. Trichology
7.Dermatohistology 17.Chemical Peeling
8.Laser epilation 18. Aesthetic Dermatology
9.Skin Surgery 19.Laser Surgery
10.Cryosurgery 20.Mesotherapy
21.Dermatoscopy
Contact information:
Address
Petrou Tcirou 35, first floor, Ap 101
PO3117
Limassol,Cyprus
Tel: 99-481008
Email:stelios.minas@telederm.org
Information for a patients

Regular examination of the skin by both you and your doctor increases the chance of finding melanoma early. Most melanomas that appear in the skin can be seen by the naked eye. Usually, there is a long period of time when the tumor grows beneath the top layer of skin but does not grow into the deeper skin layers. This period of slow growth allows time for skin cancer to be found early. Skin cancer may be cured if the tumor is found before it spreads deeper. Monthly self-examination of the skin may help find changes that should be reported to a doctor. Regular skin checks by a doctor are important for people who have already had skin cancer.
If an area on the skin looks abnormal, a biopsy is usually done. The doctor will remove as much of the suspicious tissue as possible with a local excision. A pathologist then looks at the tissue under a microscope to check for cancer cells. Because it is sometimes difficult to tell if a skin growth is benign (not cancer) or malignant (cancer), you may want to have the biopsy sample checked by a second pathologist.
Mole Mapping…..
……a safe way for early detection of Malignant melanoma.
The video documentation of moles is a safe means of skin cancer prevention.

With the aid of a video camera the dermatologist creates a mole catalogue.
This helps localize every single mole of your body.
Moles at risk are photographed individually with digital dermatoscope.
The video documentation of moles give you certainty.
The images of your moles are stored on electronic media.
The dermatologist can accurately compare earlier images to the recent ones.
EVEN THE SMALLEST CHANGE WILL BE DETECTED!!!!!
ADVANTAGE:
1.Detection of the slightest skin change
2.Dgital documentation of moles.
3.Continious mole observation
Video documentation helps the dermatologist to make the right decision and take action before it is too late!
DETECTION OF NEW MOLES WITH BODY SCAN PRO!!!
Correct skin cancer prevention must include regular check ups to see if new moles have appeared.
Body scan pro is an expert system for automatic skin checks.
This method is recommented for patients with a large number of moles.

Follow-Up Patients
Head-to-toe skin examination by a BODY SCAN PRO against the baseline record of your skin, to check for the emergence of new moles
- Repeat Digital Dermoscopic (Subsurface) and Clinical Images of all previously imaged moles
- Digital Dermoscopic and Clinical Images of any new moles + accompanying history (e.g. patient concern)
- Patient education on sun protection and self examination, including a self-monitor kit, and a CD copy of your images (upon request)
- All imaged lesions are diagnosed by Dr Stelios Minas(includes serial monitoring - comparing your most recent images with those from your previous BODY SCAN PRO to identify any subtle changes that could indicate early skin cancer. Changes that could potentially go unnoticed during a consultation with no visual history).

Medical Dermatology
The Dermatology and skin cancer clinic specializes in the diagnosis and treatment of skin, hair and nail diseases. We provide our patients and their families with full-service, comprehensive dermatologic care. We want to help you get the best of what today's medicine has to offer. And you can count on us to provide you with a smile, compassionate care and help understanding your skin condition and treatment options.
Some of the more common medical conditions we treat include acne, rosacea, cysts, moles, eczema, skin cancer detection and treatment, warts, hair loss, scalp disorders, pigmented lesions, rashes, skin allergies, nail problems, underarm sweating, vitiligo, melasma, and childhood skin diseases. As part of our preventative care, we perform very comprehensive skin checks with recommendations for full skin photography on a case-by-case basis.
We also specialize in the surgical removal of skin cancers, cysts, fatty growths and unwanted moles.

Acne
Acne vulgaris (commonly called acne) is a skin disease caused by changes in the pilosebaceous units (skin structures consisting of a hair follicle and its associated sebaceous gland). Severe acne is inflammatory, but acne can also manifest in noninflammatory forms Acne lesions are commonly referred to as pimples, blemishes, spots, zits, or acne.
Acne is most common during adolescence, affecting more than 85% of teenagers, and frequently continues into adulthood. The cause in adolescence is generally an increase in male sex hormones, which people of all genders accrue during puberty. For most people, acne diminishes over time and tends to disappear—or at the very least decrease—after one reaches his or her early twenties. There is, however, no way to predict how long it will take to disappear entirely, and some individuals will continue to suffer well into their thirties, forties and beyond.
The face and upper neck are the most commonly affected, but the chest, back and shoulders may have acne as well. The upper arms can also have acne, but lesions found there are often keratosis pilaris, not acne. Typical acne lesions are comedones, inflammatory papules, pustules and nodules. Some of the large nodules were previously called "cysts" and the term nodulocystic has been used to describe severe cases of inflammatory acne.
Aside from scarring, its main effects are psychological, such as reduced self-esteem and, according to at least one study, depression or suicide. Acne usually appears during adolescence, when people already tend to be most socially insecure. Early and aggressive treatment is therefore advocated by some to lessen the overall impact to individuals.

Rosacea
Rosacea is a common but often misunderstood condition that is estimated to affect over 45 million people worldwide. It affects mostly caucasians of mainly north-western European descent, and has been nicknamed the 'curse of the Celts' by some in Britain and Ireland, but can also affect people of other ethnicities. It begins as erythema (flushing and redness) on the central face and across the cheeks, nose, or forehead but can also less commonly affect the neck, chest, ears, and scalp.[1] As rosacea progresses, other symptoms can develop such as semi-permanent erythema, telangiectasia (dilation of superficial blood vessels on the face), red domed papules (small bumps) and pustules, red gritty eyes, burning and stinging sensations, and in some advanced cases, a red lobulated nose (rhinophyma). The disorder can be confused with, and co-exist with acne vulgaris and/or seborrhoeic dermatitis. Rosacea affects both sexes, but is almost three times more common in women, and has a peak age of onset between 30 and 60. The presence of rash on the scalp or ears suggests a different or co-existing diagnosis as rosacea is primarily a facial diagnosis, although it may occasionally appear on the scalp or ears.

Moles & Birthmarks
Known as nevi (singular ''nevus''), moles and other birthmarks are benign pigmented spots or patches of skin that range in color from tan, brown and black (moles) to red, pink or purple (vascular nevi, such as strawberry hemangiomas or port wine stains). Though most birthmarks are harmless, they may develop into cancer(Melanoma). Moles exhibiting any of the following warning signs should be examined by a professional immediately:
Larger than six millimeters -
Itches or bleeds -
Rapidly changes in color, size or shape -
Has multiple colors -
Is located where it can't be easily monitored, such as on the scalp –
High risk group: Skin cancer(Melanoma) concerns everyone,but some have a higher risk than others:
1.Patients with many pigmented lesion(The more,the higher the risk!)
2.Pigmented lesion larger than 1 cm.
3.One or more melanoma in your family
4.One or more melanoma within your own medical history
5.Severe sunburns especially during childhood or adolescence.

Skin Cancers
Skin cancer is the most prevalent of all cancers. Its main cause is over exposure to sunlight, especially sunburn. Family history is also an important risk factor. In the treatment of any skin cancers, early detection and removal is the best defence. The majority of skin cancers are preventable. As the sun is the main culprit, the most effective protection is sun avoidance. Skin cancer is a benign and malignant growth on the skin which can have many causes. The most common skin cancers are basal cell cancer, squamous cell cancer, and melanoma. Skin cancer generally develops in the epidermis (the outermost layer of skin), so a tumor is usually clearly visible. This makes most skin cancers detectable in the early stages. There are three common types of skin cancer, each of which is named after the type of skin cell from which it arises.
1. Basal Cell Carcinoma:
BCC is the most common form. The most common nodular type of BCC appears as a slowly-growing shiny white, pink or discoloured bump, most often on the face or neck. The superficial type of BCC presents as one or more irregular red scaly patches growing on the trunk or limbs.
BCC may invade into deeper tissues but does not spread to other parts of the body. Multiple BCCs are common.
2. Squamous Cell Carcinoma:
SCC is a common form of skin cancer typically found on the ear, face, lips, hands or lower legs. Invasive SCC usually grows within a solar keratosis (scaly spots due to sun damage) and presents as a tender scaly or ulcerated lump. The preinvasive phase, SCC in situ (often called Bowen's disease), characteristically presents with one or more dry or crusted red or brown patches.
Invasive SCC needs to be attended to promptly as there is a risk of secondary spread.
3. Melanoma:
The most serious form of skin cancer. Melanoma may suddenly appear without warning but it may also begin in, or near, a mole or other dark spot in the skin. For that reason it is important that we know the location and appearance of the moles on our bodies so any change will be noticed. Melanoma can spread very quickly and once it penetrates below the surface of the skin, it becomes quite deadly. That is why it is important to detect melanoma early so that you can remove it whilst it is at its thinnest and least deadly stage.

Warts
A wart (also known as verruca) is generally a small, rough tumor, typically on hands and feet but often other locations, that can resemble a cauliflower or a solid blister. Warts are common, and are caused by a viral infection, specifically by the human papillomavirus (HPV) and are contagious when in contact with the skin of an infected person. It is also possible to get warts from using towels or other objects used by an infected person. They typically disappear after a few months but can last for years and can recur.

BOTOX or botulinum toxin type A, is a protein commonly used to reduce or eliminate the appearance of facial wrinkles. It is injected under the skin into areas surrounding the eyes, forehead and mouth to smooth crow's feet, frown and worry lines, and lines on the neck.
BOTOX injections block nerve impulses, weakening muscles to relax wrinkles and give the face a rejuvenated look. BOTOX may also be useful for migraine headaches, excessive sweating, and eye and neck muscle spasms.

Chemical Peels
Chemical peels remove damaged outer layers of skin on the face to smooth texture, reduce scarring, and remove blemishes and pre-cancerous growths to produce healthy, glowing skin. There are three types of chemical peels, ranging from mild to strong - alphahydroxy acids (AHAs), tricholoroacetic acid (TCA) and phenol - and formula strengths are tailored to each patient. Peels can be combined with other procedures such as facelifts for a younger look.

Skin Fillers for Wrinkles (facial augmentation)
Facial augmentation is done for reconstructive or cosmetic purposes. It has become increasingly popular for the ‘normal’ everyday person to seek facial augmentation to remove or improve existing acne scars and facial lines or to enhance a specific facial area.
Over the years many filling (implant) agents have been developed. However, the search is still on for the ideal facial implant material. The ideal product should have the following properties:
- physiologically acceptable: incorporates itself with the body's tissues
- free of complications or side effects
- permanent: does not degrade with time
- easy to use: simple and quick procedure, e.g. injectable.
What are facial implants used for?
Facial implants can be used in reconstructions for areas that may have been scarred or altered by trauma. This may be done in conjunction with minor or major plastic surgery. The other increasing use of facial implants is in cosmetic surgery where patients seek these treatments to improve their appearance.
They are mainly used for the removal or improvement of scars caused by acne, correction of facial (wrinkle) lines, and enhancement or filling in
of certain specific facial features such as the lips or chin.
Facial lines and features that can be corrected using implants
- Frown lines (glabellar lines)
- Smoke's lines (perioral lines)
- Marionette lines (oral commissures)
- Worry lines (forehead lines)
- Crow's feet (periorbital lines)
- Deep smile lines (nasolabial furrows)
- Smile lines (nasolabial lines)
- Cheek depressions
- Lip enhancement
- Witch's chin (chin augmentation)
- Acne scars
- Facial scars

What products are available?
There are numerous implant substances that add bulk to tissue. Manufacturers of these products will claim theirs to have certain advantages over others. The decision as to which you should use will depend on what you are trying to achieve and on the expert advice of your dermatologist. Each has their place and specific uses in facial augmentation. See individual implant types for specific details regarding use.
Implant type Product names
Fat grafting
Collagen Zyderm, Zyplast, Alloderm, CosmoDerm, CosmoPlast
Hyaluronic acid Cristal,perfect,Restylane,
Hydroxyapatite Hydroxyapatite (HA), Coralline Hydroxyapatite (CH)
Silicone Popular manufacturers include Implantech, Allied Biomedical, Advanced Bio-Technologies, Inamed Aesthetics Expanded polytetrafluoroethylene (ePTFE) Gore-Tex, SoftForm
Polyethylene Medpor
Polymethyl methacrylate (PMMA) Artecoll, MetaCrill
Hydrophilic polyacrylamide Hydrogel, HPG, Argiform, Bioformacryl, DermaLive, Aquamid
Of the implant types described above, the following are injectable augmentation products:
- Collagen (excluding Alloderm®)
- Hyaluronic acid
- Polymethyl-methacrylate (PMMA)
- Hydrophilic polyacrylamide gel
These products provide facial augmentation with less downtime. Collagen and hyaluronic acid provide only a temporary solution as they are reabsorbed into the body over time; top-up treatments are necessary to maintain the desired correction. PMMA and hydrophilic polyacrylamide gel are recent additions of injectable augmentation products and claim to give more permanent results.
Are there any side effects from using facial implants?
All facial implants currently used have some side effects that preclude them from being the ideal
agent. Some of the side effects and complications that may occur include:
- allergic reactions
- bleeding and bruising
- non-allergic inflammatory reactions
- numbness
- infections
- movement or extrusion of implant

Dermatoscopy
Dermatoscopy (also known as dermoscopy or epiluminescence microscopy) is the examination of skin lesions with a dermatoscope, a magnifier with a light and a liquid medium between the instrument and the skin, thus illuminating the lesion without reflected light.
This instrument is helpful to dermatologists in distinguishing benign from malignant (cancerous) lesions, especially of aid in the diagnosis of malignant melanoma. It uses either cross-polarized or non-polarized light.

Advantages of Dermatoscopy
With doctors who are experts in the specific field of dermoscopy, the diagnostic accuracy for melanoma is significantly better than for those dermatologists who do not have any specialized training in dermatoscopy.Thus, with specialists trained in dermoscopy, there is indeed a considerable improvement in the sensitivity or detection of malignant melanomas as well as specificity or percentages of non-melanomas correctly diagnosed as compared with the traditional clinical naked eye examination.
Studies conducted have revealed that the accuracy by dermatoscopy was increased up to 20% in the case of sensitivity and up to 10% in the case of specificity.It also goes to show that detection of undiagnosed melanomas by the naked eye method is greater compared to the detection of benign lesions. By using dermatoscopy the specificity is thereby increased reducing the frequency of unnecessary surgical excisions of benign lesions.
Dermatoscopy Reduces the Need for a Biopsy. Compared to only naked eye examination in detection of melanoma conducted by dermatologists, naked eye examination coupled with dermatoscopy reduces the number of patients referred to for biopsy or excision by a significant 42%. There is a sizeable decrease in the benign-malignancy ratio of excised lesions from 18:1 where dermatoscopy is not used to 4:1 where it is used. This proves that, compared with the naked eye examination, dematoscopy not only detects melanomas more effectively but the need for unnecessary biopsy on benign lesions is considerably reduced as well.
Application of Dermatoscopy
1. The typical application of dermatoscopy is early detection of melanoma.
2. Digital dermatoscopy (videodermatoscopy) is used for monitoring skin lesions suspicious of melanoma. Digital dermatoscopy images are stored and compared to images obtained during the patient's next visit. Suspicious changes in such a lesion are an indication for excision. Skin lesions, which appear unchanged over time are considered benign.
3.Aid in the diagnosis of skin tumors - such as basal cell carcinomas, squamous cell carcinomas, cylindromas, dermatofibromas, angiomas, seborrheic keratosis and many other common skin tumors have classical dermtoscopic findings.
4. Aid in the diagnosis of scabies and pubic louse. By staining the skin with india ink, a dermatoscope can help identify the location of the mite in the burrow, facilitating scraping of the scabetic burrow. By magnifying pubic louse, it allows for rapid diagnosis of the difficult to see small insects.
5. Aid in the diagnosis of warts. By allowing a physician to visualize the structure of a wart, to distinguish it from corn, callouses, trauma, or foreign bodies. By examining warts at late stages of treatment, to assure that therapy is not stopped prematurely due to difficult to visualize wart structures.
6. Aid in the dianosis of fungal infections. To differentiate "black dot" tinea, or tinea capitis (fungal scalp infection) from alopecia areata.
7. Aid in the diagnosis of hair and scalp diseases, such as alopecia areata , female androgenic alopecia, monilethrix Netherton syndrome, and woolly hair syndrome. Dermoscopy of hair and scalp is called trichoscopy.
8. Determination of surgical margin of hard to define skin cancers. Examples would be Bowen's disease, superficial basal cell carcinomas, and lentigo malignas. These tumors have very indistinct margins. By allowing the surgeon to correctly identify the true extent of the tumor, repeat surgery often is decreased.

Mesotherapy
Mesotherapy (from Greek mesos, "middle", and therapy from Greek therapeia, "to treat medically") is a non-surgical cosmetic medical treatment.
Pioneered by the French physician Dr. Michel Pistor in 1952, Mesotherapy is a minimally invasive procedure that is widely used in Europe and elsewhere to treat various injuries and medical conditions. This medical specialty targets problem areas with microinjections of conventional or homeopathic medicines, vitamins, minerals and amino acids. Tiny "medicinal bullets" are delivered directly into the mesoderm (middle layer of skin) that are highly specific to the condition being treated. Among its many applications, Mesotherapy can be used for the following:
- Mesotherapy to eliminate cellulite
- Mesotherapy to promote weight loss
- Mesotherapy to provide anti-aging benefits
- Mesotherapy to eliminate localized fat deposits
Mesotherapy ( Mesotherapie) was recognized by the French National Academy of Medicine in 1986 as an integral part of traditional medicine. Each day, thousands of doctors worldwide use Mesotherapy to help tens of thousands of patients.

Laser hair removal
Epilation by laser was performed experimentally for about 20 years before it became commercially available in the mid 1990s. One of the first published articles describing laser hair removal was authored by the group at Massachusetts General Hospital in 1998. The efficacy of laser hair removal is now generally accepted in the dermatology community, and laser hair removal is widely practiced. Many reviews of laser hair removal methods, safety, and efficacy have been published in the dermatology literature.
Mechanism of action
The primary principle behind laser hair removal is selective photothermolysis (SPTL). Lasers can cause localized damage by selectively heating dark target matter, (melanin), in the area that causes hair growth, (the follicle), while not heating the rest of the skin. Light is absorbed by dark objects, so laser energy can be absorbed by dark material in the skin (but with much more speed and intensity). This dark target matter, or chromophore, can be naturally-occurring or artificially introduced.
Hair removal lasers selectively target melanin:
- Melanin is considered the primary chromophore for all hair removal lasers currently on the market. Melanin occurs naturally in the skin (it gives skin and hair its color). There are two types of melanin in hair: eumelanin (which gives hair brown or black color) and pheomelanin (which gives hair blonde or red color). Because of the selective absorption of photons of laser light, only black or brown hair can be removed.
Both men and women seek laser hair removal services to have superfluous or unwanted hair removed. Hair removal is commonly done on lip, chin, ear lobe, shoulders, back, underarm, abdomen, buttocks, pubic area, bikini lines, thighs, face, neck, cleavage, chest, arms, legs, hands, and toes.
Laser works best with dark coarse hair. Light skin and dark hair are an ideal combination, but new lasers are now able to target dark black hair even in patients with dark skin.
Hair removal lasers have been in use since 1997 and the Food and Drug Administration approved it for “permanent hair reduction.” Laser hair removal has become extremely popular because of its speed and efficacy, although some of the efficacy is dependent upon the skill and experience of the laser operator, and the choice and availability of different laser technology at the clinic which is performing the procedure. Some will need touch-up treatments, especially on large areas, after the initial set of 3-8 treatments. It has also been observed that some people seem to be non-responders – this is not confirmed and reasons are not known, and may in fact be due to lack of skill on the part of many laser operators and/or the type of machine and settings they are using.
Laser parameters that affect results
Several wavelengths of laser energy have been used for hair removal, from visible light to near-infrared radiation. These lasers are usually defined by the lasing medium used to create the wavelength (measured in nanometers (nm)):
- Argon: 488 or 514.5 nm (no longer used for hair removal)
- Ruby: 694 nm (no longer used for hair removal; not safe on most skin types as it frequently produces side effects such as pigmentary changes (lightening or darkening of the skin) or worse for patients of all but white skin.
- Alexandrite: 755 nm (most effective, but safest on light skin)
- Pulsed diode array: 810 nm (for light to medium type skin)
- Nd:YAG: 1064 nm (for darker skin; Yag is capable of treating all six skin colors. However, there is not sufficient evidence that this laser can produce effective long-term hair removal)


Cryosurgery
Cryosurgery (cryotherapy) is the application of extreme cold to destroy abnormal or diseased tissue. The term comes from the Greek words cryo (κρύο) ("icy cold") and surgery (cheirourgiki - χειρουργική) meaning "hand work" or "handiwork". Cryosurgery is used to treat a number of diseases and disorders, especially a variety of benign and malignant skin conditions.
Warts, moles, skin tags, solar keratoses, and small skin cancers are candidates for cryosurgical treatment. Several internal disorders are also treated with cryosurgery, including liver cancer, prostate cancer, cervical disorders and, more commonly in the past, hemorrhoids. Although found to be effective, this method of treatment is only appropriate for use against localized disease with no metastasis.
Cryosurgery works by taking advantage of the destructive force of freezing temperatures on cells. At low temperatures, ice crystals form inside the cells, which can tear them apart. More damage occurs when blood vessels supplying the diseased tissue freeze.
The most common method of freezing lesions is using liquid nitrogen as the cooling solution. The super-cooled liquid may be sprayed on the diseased tissue, circulated through a tube called a cryoprobe, or simply dabbed on with a cotton or foam swab. Less frequently, doctors use carbon dioxide "snow" formed into a cylinder or mixed with acetone to form a slush that is applied directly to the treated tissue. Recent advances in technology have allowed for the use of argon gas to drive ice formation using a principle known as the Joule-Thomson effect. This gives physicians excellent control of the ice, and minimizing complications using ultra-thin 17 gauge cryoneedles.
Cryosurgery is a minimally invasive procedure, and is often preferred to more traditional kinds of surgery because of its minimal pain, scarring, and cost; however, as with any medical treatment, there are risks involved, primarily that of damage to nearby healthy tissue. Damage to nerve tissue is of particular concern.
Patients undergoing cryosurgery usually experience minor-to-moderate localized pain and redness, which can be alleviated by oral administration of an analgesic such as aspirin, ibuprofen or acetaminophen (paracetamol). Blisters may form, but these usually scab over and peel away within several days.